United Kingdom Digital Health Market Analysis by Mordor Intelligence
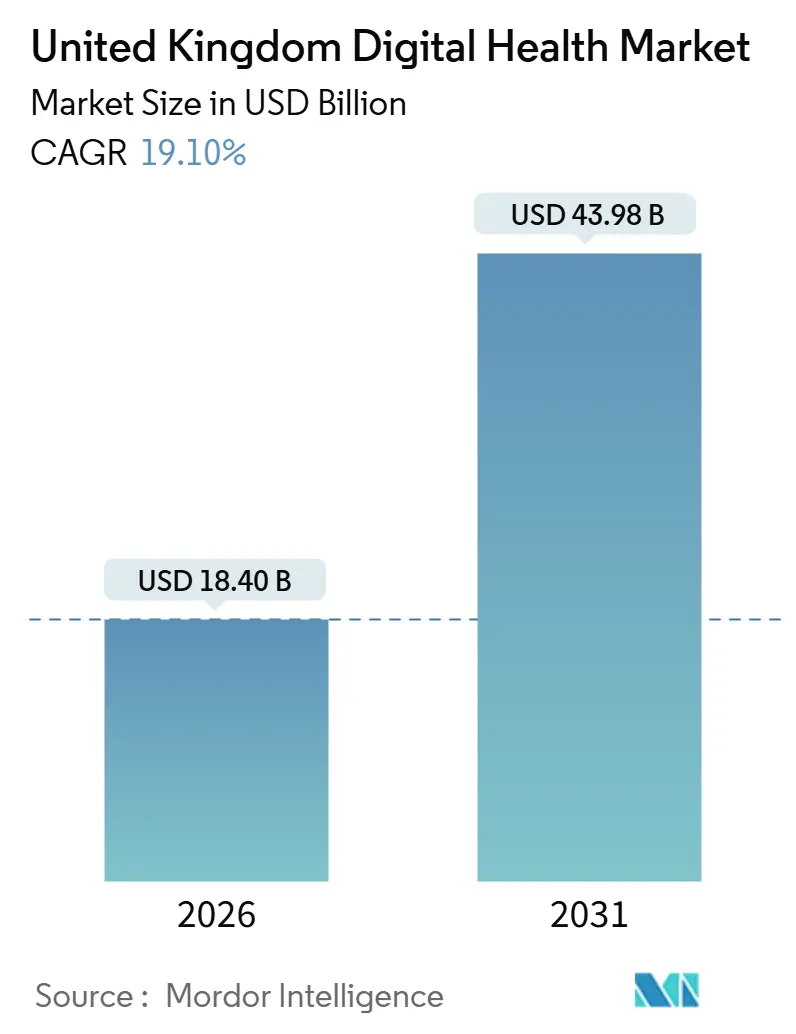
The United Kingdom digital health market size is expected to reach USD 18.40 billion in 2026 and is projected to reach USD 43.98 billion by 2031, reflecting a CAGR of 19.10% over 2026-2031. Driving forces include sustained National Health Service (NHS) investment in electronic patient records (EPRs), fast-growing virtual ward capacity, the expanding user base of the NHS App, and an emerging wave of AI-enabled analytics that optimizes care pathways while reducing administrative burden. Incumbent vendors defend entrenched software estates, yet cloud-native challengers use data-platform contracts to seed adjacent analytic and workflow tools, fragmenting the competitive field. Procurement frameworks that deliberately favor multivendor awards create openings for smaller suppliers with specialized capabilities, while cybersecurity incidents and interoperability gaps temper near-term hardware demand and elevate cloud migration as a lower-risk alternative. In parallel, carbon-reduction mandates force providers and vendors to favor energy-efficient architectures, a shift that reinforces the long-term pivot toward hyperscale cloud hosting and software-as-a-service delivery.
Key Report Takeaways
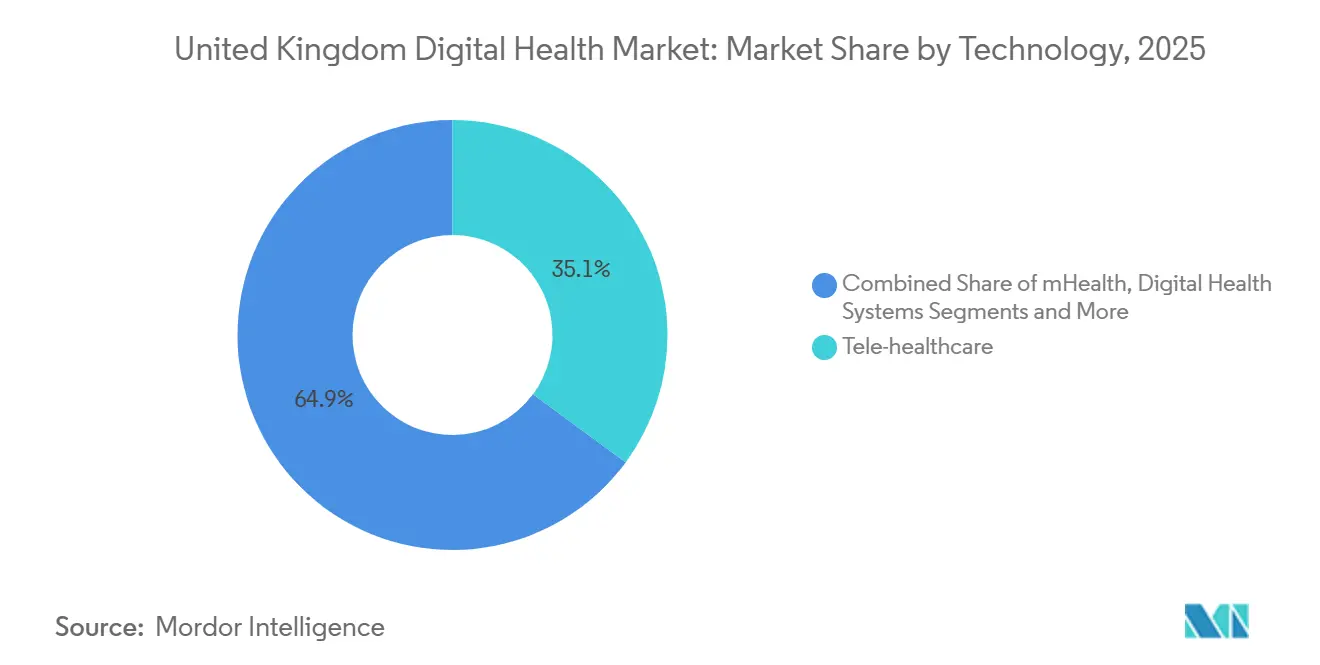
- By technology, Tele-Healthcare led with 35.1% revenue share in 2025; Healthcare Analytics & AI is forecast to advance at a 19.8% CAGR through 2031.
- By component, Software accounted for 59.1% of the United Kingdom digital health market share in 2025, while services are expected to show the highest projected CAGR at 20.3% during 2026-2031.
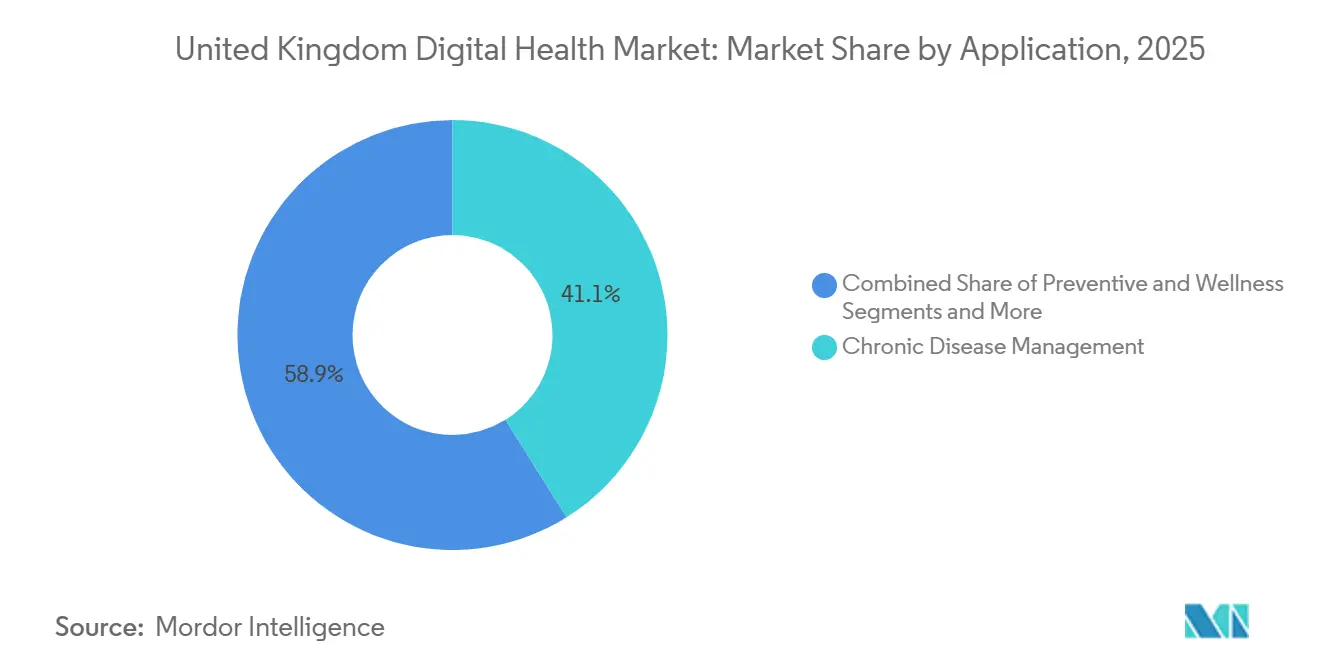
- By application, Chronic Disease Management captured 41.1% of 2025 spend; Diagnostics & Decision Support is set to expand at a 21.2% CAGR to 2031.
- By end-user, Hospitals & NHS Trusts represented 60.4% of expenditure in 2025, whereas Patients/Home-Care Settings are growing at 20.6% CAGR through 2031.
Note: Market size and forecast figures in this report are generated using Mordor Intelligence’s proprietary estimation framework, updated with the latest available data and insights as of January 2026.
United Kingdom Digital Health Market Trends and Insights
Drivers Impact Analysis
| Driver | (~) % Impact on CAGR Forecast | Geographic Relevance | Impact Timeline |
|---|---|---|---|
| NHS Long-Term Digital Funding Commitments | +4.2% | England (primary), Scotland, Wales, Northern Ireland | Medium term (2-4 years) |
| Accelerating EPR Roll-Outs Across Secondary Care | +3.8% | England acute trusts, Scotland regional boards, Wales health boards | Short term (≤2 years) |
| Majority of Population’s Monthly Use Target for NHS App | +3.1% | UK-wide | Medium term (2-4 years) |
| Expansion of Virtual Wards & Remote Monitoring | +3.5% | England ICSs, Scotland, Wales | Short term (≤2 years) |
| Federated Data Platform-Enabled AI “App-Store” Ecosystem | +4.6% | England (national), pilots in Scotland and Wales | Long term (≥4 years) |
| Source: Mordor Intelligence | |||
NHS Long-Term Digital Funding Commitments
NHS England’s GBP 13.4 billion digital transformation allocation through 2025 created a predictable procurement pipeline that underpinned vendor investment, allowing trusts to replace patient-administration systems averaging 15 years of age in 2020 with software only eight years old by 2025[1]NHS England, “Virtual Wards Programme,” england.nhs.uk. Scotland added GBP 300 million and NHS Wales GBP 200 million for comparable programs, producing parallel opportunities for suppliers capable of multi-jurisdiction deployment. Front-loaded funding compressed implementation timetables, increasing demand for managed-service partners that can absorb short-term staffing peaks.
Accelerating EPR Roll-Outs Across Secondary Care
EPR coverage in English acute trusts rose from 43% in 2023 to an anticipated 80% by mid-2026, propelled by elective-recovery incentives and integrated care system (ICS) maturity metrics. Oracle Health’s Millennium went live at Newcastle Hospitals under a GBP 32.5 million deal, and a multi-trust London deployment consolidated three standalone records into one, illustrating economies of scale in larger footprints. Early adopters are now layering population-health analytics onto mature data sets, widening capability gaps between digital leaders and late adopters.
Majority of Population’s Monthly Use Target for NHS App
The NHS App reached 36 million users by June 2025, equal to 54% of U.K. adults. Added functionality such as vaccination booking, organ-donation registration, and NHS 111 triage extends the app’s utility, reducing call-center workload by 20% in high-adoption practices. Usage skews toward digitally literate patients; only 18% of over-65s are active users, indicating that broader impact requires assisted-digital programs targeting older cohorts.
Expansion of Virtual Wards & Remote Monitoring
Virtual-ward capacity exceeded 10,000 beds by late-2024, and NHS England targets 15,000 beds by 2027. Remote-monitoring platforms capture oxygen saturation, heart rate, and blood pressure, escalating deteriorating cases for early intervention while converting fixed-estate cost into variable technology spend. Connectivity gaps caused 12% of monitoring lapses during a 2025 audit, highlighting infrastructure fragility in rural regions [2]National Audit Office, “Virtual Wards Audit Report,” nao.org.uk.
Restraints Impact Analysis
| Restraint | (~) % Impact on CAGR Forecast | Geographic Relevance | Impact Timeline |
|---|---|---|---|
| Cyber-Security & Data-Privacy Concerns | -1.8% | UK-wide | Short term (≤2 years) |
| Interoperability Gaps in Legacy NHS IT | -1.5% | England acute trusts, Scotland boards, Wales boards | Medium term (2-4 years) |
| Clinician “Shadow-IT” Workarounds | -1.2% | UK-wide | Medium term (2-4 years) |
| Rising Carbon-Reduction Compliance Costs | -0.9% | UK data-center estates | Long term (≥4 years) |
| Source: Mordor Intelligence | |||
Cyber-Security & Data-Privacy Concerns
Ransomware disrupted several trusts in 2024-2025, forcing temporary reliance on paper records and delaying elective procedures [3]National Cyber Security Centre, “Cyber Security Incidents in Healthcare,” ncsc.gov.uk. Annual Data Security and Protection Toolkit assessments now require trusts to exceed baseline cyber-maturity standards, adding GBP 0.5 million-2 million in annual compliance costs. Extended procurement due-diligence cycles particularly strain smaller vendors that lack formal security certifications.
Interoperability Gaps in Legacy NHS IT
A 2025 Royal College of Physicians survey found 68% of clinicians still re-enter data when handing off patients between primary and secondary care. Coexistence of HL7 v2, FHIR, and proprietary APIs forces middleware deployments that multiply points of failure and inflate technical debt. Mandatory adoption of FHIR UK Core will take several years to retrofit across installed systems.
Segment Analysis
By Technology: AI and Analytics Outpace Legacy Tele-Health
Healthcare Analytics & AI is projected to grow at a 19.8% CAGR, outstripping the mature Tele-Healthcare segment that held a 35.1% share of the United Kingdom digital health market in 2025. Trusts redirect budgets from pandemic-era video-consultation tools to predictive analytics that forecast emergency-department volumes and allocate staff accordingly, demonstrated by 85% prediction accuracy in early FDP pilots. Tele-Healthcare remains essential for GP and specialist consultations but faces slower incremental growth as adoption reaches saturation in urban areas.
The digital health systems layer, dominated by Oracle Health and Epic, anchors hospital workflows, while remote monitoring & wearables gain momentum through virtual-ward expansion. mHealth applications, epitomized by the NHS App, provide a ubiquitous patient front door yet generate lower revenue per user than AI-powered analytics. Data-platform apps built on the FDP create a marketplace that diffuses innovation across multiple vendors instead of consolidating power within EPR incumbents.
Note: Segment shares of all individual segments available upon report purchase
By Component: Services Surge as Integration Complexity Mounts
Software licenses and SaaS subscriptions delivered 59.1% of United Kingdom digital health market revenue in 2025, but Services implementation, integration, and managed support are forecast to rise at a 20.3% CAGR through 2031, almost matching overall market growth. Migration from legacy databases, workforce training, and ongoing interoperability maintenance drive sustained demand for professional services long after initial go-lives.
Infosys’s GBP 1.17 billion Electronic Staff Record contract exemplifies bundled software-plus-services engagements that transfer operational risk to the vendor. Hardware sales shrink as trusts shift workloads to hyperscale cloud platforms. Service providers also absorb the cost of retrofitting HL7 interfaces to FHIR and decommissioning shadow-IT workarounds, reinforcing their strategic role throughout the transformation cycle.
By Application: Diagnostics AI Gains as Chronic Care Plateaus
Chronic Disease Management retained 41.1% of 2025 spending, but growth moderates as diabetes and cardiovascular programs near coverage saturation in major ICSs. Diagnostics & Decision Support leads future expansion with a 21.2% CAGR, catalyzed by AI algorithms that prioritize images for radiologist review and cut reporting backlogs.
Preventive & Wellness apps remain underfunded, absorbing less than 8% of spend despite policy emphasis on prevention. Administration & Workflow Automation grows steadily, highlighted by AI-based clinical-note tools that reduce documentation time by 40%. Mental health, precision medicine, and virtual care carve smaller but rising allocations as reimbursement models scale.
Note: Segment shares of all individual segments available upon report purchase
By End-User: Home-Care Settings Accelerate as Hospitals Consolidate
Hospitals & NHS Trusts held 60.4% of 2025 spending, anchored by EPR roll-outs, yet growth slows as roll-out waves crest and budgets shift toward optimization. Patients/Home-Care Settings lead future expansion with a 20.6% CAGR, driven by wearables and virtual wards that relocate monitoring to living rooms.
Primary Care & GP Practices gain purchasing autonomy through the GBP 400 million Digital Services Framework, encouraging workflow and decision-support pilots that challenge historical incumbents. Payers & Commissioners wield indirect power by linking funding to digital-maturity criteria, effectively mandating EPR and interoperability compliance across provider networks.
Geography Analysis
England comprises the bulk of the United Kingdom's digital health market spend by virtue of its population and centrally managed NHS England procurement programs. Forty-two ICSs function as semi-autonomous purchasers, and early FDP pilots in five of them provide reference deployments that neighboring regions often emulate. Scotland’s GBP 300 million Digital Health & Care Strategy funds a national shared-care record that minimizes vendor fragmentation but increases platform risk if deployments falter.
Wales pursues a Once for Wales single-platform model that awarded an EPR contract in 2024, while Northern Ireland leverages its combined health-and-social-care structure to trial unified clinical and social-care workflows. Rural broadband deficits below 10 Mbps limit video consultations and remote monitoring in parts of Scotland, Wales, and Northern Ireland, an issue the UK Government’s Project Gigabit aims to resolve by 2030.
Interstate patient flows expose interoperability gaps: only 60% of Scottish acute hospitals ran modern EPRs by mid-2025 versus 80% in England, complicating data exchange when patients cross borders for specialist services. Vendors that secure flagship deployments in high-population English ICSs frequently leverage those references to win contracts in smaller devolved markets, reinforcing a first-mover advantage.
Competitive Landscape
EPR and primary-care software remain moderately concentrated, with two vendors covering the majority of GP practices, yet no single supplier exceeds 15% share in the rapidly expanding AI analytics, remote monitoring, or virtual-care niches. High switching costs and data-network effects help incumbents retain hospitals that invested GBP 20 million-50 million per deployment, but cloud-native entrants sidestep entrenched systems by offering adjacent analytic or workflow tools that integrate via open APIs.
NHS procurement policy now encourages fragmentation: the 2026 Primary Care Digital Services Framework split GBP 400 million across 12 vendors, lowering entry barriers for specialized suppliers. Global platform providers pursue multi-tens-of-millions acute trust deals, while U.K.-native companies focus on task-specific SaaS offerings that scale rapidly through low-friction adoption models. Regulatory requirements such as the Digital Technology Assessment Criteria favor vendors with established compliance processes, subtly disadvantaging early-stage startups.
United Kingdom Digital Health Industry Leaders
EMIS Health (Optum)
TPP (SystmOne)
Cerner (Oracle Health)
Epic Systems
Alcidion
- *Disclaimer: Major Players sorted in no particular order
Recent Industry Developments
- June 2025: UK Government committed up to GBP 10 billion for NHS technology and digital transformation through 2029.
- May 2025: A joint GBP 600 million initiative with Wellcome Trust launched the by UK Health Data Research Service.
- January 2025: “A Blueprint for Modern Digital Government” set a six-point plan that includes AI integration and a GOV.UK App.
Research Methodology Framework and Report Scope
Market Definitions and Key Coverage
Our study views the United Kingdom digital health market as every clinically oriented software, connected device, and data-analytics service that supports remote or in-facility diagnosis, treatment, monitoring, or workflow. This includes tele-healthcare platforms, mHealth applications, electronic patient records, remote patient-monitoring hardware, and healthcare analytics solutions procured by the NHS, private providers, payers, and consumers. According to Mordor Intelligence, the market stands at USD 15.46 billion in 2025 and is projected to reach USD 36.84 billion by 2030.
Scope exclusion: stand-alone fitness trackers or wellness apps lacking regulated clinical utility are left outside this assessment.
Segmentation Overview
- By Technology
- Tele-Healthcare
- mHealth Applications
- Digital Health Systems (EPR, PAS, Shared-Care Records)
- Healthcare Analytics & AI
- By Component
- Software
- Hardware
- Services
- By Application
- Chronic Disease Management
- Preventive & Wellness
- Diagnostics & Decision Support
- Administration & Workflow Automation
- Mental & Behavioural Health
- Genomics & Precision Medicine
- Virtual Care & Hospital-at-Home
- By End-User
- Hospitals & NHS Trusts
- Primary Care & GP Practices
- Patients / Home-Care Settings
- Payers & Commissioners (ICBs, NI HSC, NHS Wales, NHS Scotland)
Detailed Research Methodology and Data Validation
Primary Research
Mordor analysts interview NHS procurement leads, digital-health clinicians, private tele-care operators, insurers, and patient-led advocacy groups across England, Scotland, Wales, and Northern Ireland. These engagements confirm adoption rates, average selling prices, implementation timelines, and reimbursement shifts that secondary data alone cannot capture.
Desk Research
We begin with an extensive desk review of high-credibility, non-paywalled sources such as NHS Digital activity dashboards, Office for National Statistics health expenditure tables, Medicines & Healthcare products Regulatory Agency device registries, OECD Health Data, and World Health Organization eHealth indicators. Company filings, investor decks, reputable press, and selective pulls from D&B Hoovers and Dow Jones Factiva enrich financials and competitive moves. Diverse customs logs and patent counts are tapped when device import volume or innovation cadence influences demand signals. The sources named illustrate the breadth; many additional references inform data collection and validation.
Market-Sizing & Forecasting
A top-down reconstruction from national health spending and digital-care penetration rates sets the market pool, which is then sense-checked with selective bottom-up supplier roll-ups and ASP × unit snapshots. Key variables like virtual-ward bed capacity, smartphone penetration, EPR deployment progress, chronic-disease prevalence, and public AI investment drive annual value adjustments. Multivariate regression produces the 2025-2030 forecast, while gap patches in micro-segments are bridged through calibrated proxies or expert consensus.
Data Validation & Update Cycle
Model outputs undergo variance checks against independent metrics before a senior review panel signs off. Reports refresh yearly, and analysts trigger interim revisions when material events alter baseline assumptions.
Why Mordor's United Kingdom Digital Health Baseline Earns Trust
Published estimates often diverge because firms apply different scopes, input sources, and refresh cadences.
Key gap drivers include: some publishers bundling wellness wearables, others using global price averages without NHS discounting, or projecting straight-line uptake rather than our scenario-tested adoption curves.
Benchmark comparison
| Market Size | Anonymized source | Primary gap driver |
|---|---|---|
| USD 15.46 B (2025) | Mordor Intelligence | - |
| USD 12.80 B (2024) | Global Consultancy A | Excludes analytics services; older base year |
| USD 10.65 B (2024) | Research Publisher B | Uses retail ASPs, omits NHS bulk-buy discounts |
| USD 12.82 B (2024) | Analytical Firm C | Assumes uniform 20% CAGR without device-service mix shifts |
The comparison shows that once scope alignment, price realism, and yearly recalibration are applied, Mordor's numbers provide a balanced, transparent baseline that decision-makers can trace back to explicit variables and repeatable steps.
Key Questions Answered in the Report
How big will be the UK digital health market in 2026?
The UK digital health market size is expected to reach USD 18.40 billion in 2026 and is forecast to expand at a 19.10% CAGR through 2031.
Which technology segment is growing fastest?
Healthcare Analytics & AI leads growth, advancing at a 19.8% CAGR on the back of predictive models and AI-driven decision support.
What share do hospitals hold in overall spending?
Hospitals and NHS Trusts account for 60.4% of 2025 spending, though home-care settings are expanding more quickly
How many users are on the NHS App?
The NHS App registered 36 million users by mid-2025, covering more than half of the U.K. adult population
What is the biggest restraint on adoption?
Cyber-security and data-privacy concerns remain the foremost barrier, with ransomware adding cost and slowing procurement cycles.